COVID-19 vaccine hesitancy: How to overcome the culture of mistrust
February 4, 2021

Two COVID-19 vaccines that offer nearly 95 percent protection against the virus have been developed, approved, and delivered in less than a year. For the scientific community, that’s the equivalent of scaling Mount Everest in a day.
But there are other steep mountains left to climb.
Building confidence in those vaccines, breaking through layers of mistrust, and persuading the majority of the public to get vaccinated could prove even more challenging.
In a recent Associated Press poll, only about half of Americans said they will get vaccinated, and those numbers were significantly lower among Black (24 percent) and Hispanic (34 percent) respondents. Considering that the COVID-19 death rate for Black, Latino, and Native American populations is 2.7 times higher than it is among white Americans, that is especially concerning.
“Vaccine hesitancy” is a complex condition – recognized as a top 10 threat to global health by the World Health Organization in 2019. As a UT Southwestern infectious diseases specialist who also treats patients at Parkland Hospital, I have seen the effects of this public health issue up close and have devoted much of my research to developing solutions for it.
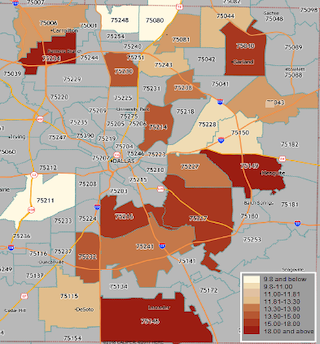
Over the last year, my team at the Center for Innovation and Value at Parkland Hospital partnered with Dallas County Health and Human Services (DCHHS) to pilot a community-engaged influenza vaccine effort in a ZIP code (75217) identified by the Community Needs Health Assessment (CHNA) as having multiple health disparities – including twice the age-adjusted mortality rate for influenza and pneumonia compared with other parts of Dallas.
The pilot was conducted in a largely Hispanic community utilizing local high school students to co-create and disseminate culturally specific flu vaccine information via sources of trust, such as local churches and Spanish-language radio stations. Following the success of the first event, we conducted focus groups with community members and expanded the role of health ambassadors to attain a broader reach in October 2020. We subsequently piloted the program with students from South Oak Cliff High School in a predominantly Black community ZIP code (75216).
Over the course of four events and 16 hours, we vaccinated approximately 1,300 individuals – many uninsured and without a “medical home.” The lessons we learned could provide a valuable road map for countering the effects of vaccine hesitancy surrounding the COVID-19 vaccines. In short, the messages should be:
- The COVID-19 vaccines are safe and very effective.
- Your community is at increased risk for COVID-19 complications.
- Vaccines will protect you, your family, and your neighbors.
- Many doctors, nurses, and community leaders have already received the vaccines.
- Despite past abuses, these vaccines are our best chance to end the pandemic.
With the right message and the right messengers, we can prevent people from dying from a virus that is now preventable.
Building a culture of health, trust
Vaccines are among the most impactful medical advances in our history, credited with saving more than 1 billion lives. Yet a multitude of factors – political, religious, racial, educational, and systemic – have given rise to a growing culture of uncertainty about these medical discoveries.
Dark and tragic episodes from the past, such as the Tuskegee syphilis study, remain deeply rooted in the consciousness of minority communities. In the 40-year experiment, Black men were misled about the research and forced to suffer from untreated syphilis, despite the availability of penicillin. Present-day problems, such as the lack of access to adequate health care and insurance, persist in minority communities.
In January 2020, we partnered with students at Cristo Rey College Prep School who were interested in careers in medicine – our “health ambassadors” – to develop a culturally specific pilot program to see if we could improve flu vaccination rates in their predominantly Hispanic neighborhood. When we met with the students initially, we shared a Community Health Needs Assessment map, which clearly showed that people in their home ZIP code suffered severe illness and death from influenza at much higher rates than people in nearby areas in North Texas. Seeing the darkly shaded region where they reside contrasted with other areas on the map, one high school student remarked: “That’s health segregation.”
The data compelled them to spread the message to their parents, extended families, and their community that vaccines saves lives.
Through a generous donation to UT Southwestern’s endowment fund, which was earmarked to help medically underserved populations, we were able to create a program, messaging campaign, and several events that connected with the community:
- The students recorded radio spots and we bought airtime on the most popular Spanish-language stations in the area to spread the word about the events.
- Flyers created by the students were posted at businesses, schools, and churches around the neighborhood.
- St. Augustine Catholic Church became a forum for trust, helping create buy-in for the first event in the church parking lot.
- More than two-thirds of the participants completed a post-immunization survey, which helped us collect data and gain a better understanding of attitudes and perceptions of the influenza vaccine.
Among the 400 people attending the first vaccination event, more than 40 percent reported not receiving a flu shot the year before. Many had never had a flu shot. Throughout the first 10 months of 2020, we vaccinated more than 1,300 people over 16 hours at four community-led events in Pleasant Grove and South Oak Cliff.
The student health ambassadors became effective and crucial influencers in their communities. We will need to enlist the help of younger generations and this community-engaged approach again as we try to counter reluctance toward the new, scientifically sound COVID-19 vaccines.
Bridging the gaps
There is no one-size-fits-all answer to the question: “Why should I get vaccinated?” But we can build a culture of trust if we start at the grassroots level, listening to people’s concerns and understanding the origins of their hesitation.
During our pilot programs, we surveyed hundreds of people who had never been vaccinated before. Their responses sent a clear message that mistrust, misinformation, and inequalities in our government and health care institutions all contribute to this global problem.
Here are five of the most common concerns we heard, and some potential responses to allay fears about vaccines.
1. How do I know you’re not experimenting on me?
The horrors of Tuskegee and stories of forced sterilizations in some minority communities remain top of mind. Immigration policies also sow distrust among undocumented residents. By empowering our health ambassadors with the facts about vaccine efficacy, as well as health statistics and mortality rates in their community, they can make inroads with their parents and family members.
For the COVID-19 vaccine, it might also be of interest to note that Dr. Kizzmekia Corbett, an African-American scientist with the National Institutes of Health, was instrumental in developing the Moderna vaccine. (Dr. Corbett will be the featured speaker Feb. 10 at a UT Southwestern science and medicine lecture series.) Many of UT Southwestern’s physicians, nurses, and hospital employees of color have also been outspoken about the benefits and safety of the vaccines, with some posting photos of their COVID-19 vaccinations on social media.
Seeing positive representations in the science and medical communities can be an effective way to ease worries about past inequities and abuses.
Some vaccine hesitancy is rooted in history and culture
Dr. Kavita Bhavan says it's important to acknowledge how abuses and inequities in the past, such as the Tuskegee syphilis study, continue to play a role in a culture of vaccine hesitancy today.
2. Is the vaccine going to give me COVID-19 or alter my DNA?
The two COVID-19 vaccines currently approved for emergency use do not contain any form of the virus, so there is no risk of it causing the disease. The Pfizer-BioNTech and Moderna vaccines both use messenger RNA (mRNA), which is a synthetic genetic code, to provoke an immune response. The mRNA never enters the nucleus of the cell, which is where DNA lives, so it does not affect a person’s DNA.
Many vaccines use a weakened or inactive version of a virus to stimulate an immune response. This is true for the flu vaccine and it is a safe scientific practice. But persistent misinformation has convinced some people that vaccines will make them sick.
3. How do I know steps were not skipped to produce these vaccines quickly?
Mistrust of government officials, pharmaceutical companies, and medical experts feeds vaccine hesitancy and some conspiracy theories. For instance, a video shared on social media falsely claimed that some vaccines include an optional microchip that will be injected into patients to allow the government to track them. It was later revealed that the video of a scientist was edited to falsely give that impression.
So, it’s important to share verifiable facts. The COVID-19 vaccines, for instance, followed a well-established clinical trial regimen that is required by the Food and Drug Administration for any new drug seeking authorization. If you take medication for diabetes or high blood pressure, those drugs were put through the same process. The only difference with COVID-19 vaccines is the wait times for independent reviews of the testing data were accelerated – essentially, they cut through the red tape to get the vaccines ready for the public sooner because of the pandemic. The manufacturing and distribution processes were also created as the clinical trials were ongoing so that if/when the vaccines were approved, the companies would be ready to distribute the vaccines without delay.
Bottom line? No steps were skipped, and safety was not sacrificed for speed.
UT Southwestern also assembled its own panel of experts to independently review the vaccine trial and safety data and deemed both vaccines safe and highly effective.
4. If the vaccine is so effective, why is it free?
In our pilot program, we emphasized that flu vaccines were free because we know medical costs can be a deterrent for some patients. But several respondents from our Spanish-speaking focus group said “free” also has the potential to signal to people in their community that the vaccine is ineffective or outdated. “If it’s free, it must not work,” they said.
Emphasizing the vaccine’s connection to a familiar medical institution, such as Parkland, might be a more effective way to enhance its credibility, they suggested. No-cost vaccines, paid for by Operation Warp Speed, represent a benefit to many patients. But the government’s involvement can raise a red flag for others. Developing messaging that explains COVID-19 vaccines are supported by a federal program because the country is facing a public health crisis – and it is vital that everyone gets vaccinated – can also help limit skepticism.
'Free' vaccines can carry a stigma
In the flu vaccine pilot program, Dr. Bhavan and her team emphasized that vaccines were free. But several participants said that message had an unintended negative connotation for them. 'Free' vaccines suggested to some in the largely Hispanic neighborhood that they didn't work or were outdated.
5. Why should I be among the first to get vaccinated?
Nearly 40 percent of Americans are taking a wait-and-see approach to the COVID-19 vaccines, according to recent polls, and that mindset likely comes from a combination of factors:
- Many people experience mild or moderate symptoms from COVID-19, so they view the virus as a hypothetical risk – until it hits close to home. But more than 450,000 Americans have died from COVID-19 in less than a year, and in early January the death toll topped 4,000 people per day.
- The vaccines are new, and while they’ve been proven safe and nearly 95 percent effective in clinical trials, we don’t have years of data on them yet.
- Vaccine supply is limited and not yet available to everyone in the general public.
Though the vaccine supply is limited at the moment, it’s important to begin persuading people now who are hesitant about vaccination, so they’ll be ready when it is available to them. The best way to do that is by emphasizing tangible benefits:
- By protecting yourself and your family members from the virus, you can begin to relax and return to having gatherings with vulnerable relatives, especially after they are all vaccinated.
- People in communities of color are dying at disproportionately high rates. Share the COVID-19 data – it makes a compelling case for vaccination.
- If you don’t have access to good health care, you may not know if you have underlying conditions that could increase your risk for severe complications from COVID-19, such as diabetes or cardiovascular disease. It’s not worth taking that risk when safe and effective vaccines are becoming available.
- Finally, you have to weigh the risks of getting the vaccine, which are minor, with not getting it. Yes, the COVID-19 vaccines may have some mild side effects – arm soreness at the injection site; fatigue, chills, or headaches for a day or two are possible. But the risk of COVID-19 infection can be much more severe and long-lasting. A recent study showed that three-quarters of people hospitalized for COVID-19 complications were still experiencing symptoms six months after infection.
Building confidence in the COVID-19 vaccines
Dr. Quinn Capers, Associate Dean for Faculty Diversity at UT Southwestern and a national leader on the issue of diversity and inclusion in medicine, discusses the keys to delivering a message of trust on the vaccines to Black and Hispanic patients.
Final thoughts on an uphill climb
As an infectious disease specialist, I’ve found the key to having a productive conversation about the COVID-19 vaccines is trying to understand the patient's concerns and fears. Don’t dismiss them. Listen.
For some people the science, facts, and data will persuade them that getting vaccinated is the right choice. Others will need more assurances because you may be asking them to set aside long-held cultural beliefs. Those assurances could come from within their own family – maybe even a future physician or scientist.
When it comes to COVID-19 vaccines, it’s not enough to just get the science right. The message matters, and so does the messenger.
“It’s a challenge,” Jasmine Ramirez, one of our health ambassadors, told a reporter covering our event in Pleasant Grove. “Many people are scared about the side effects. They want to see a familiar face (when they get vaccinated), and they want to see people that care about them as well.”
Building and restoring trust in medical systems and health interventions require a commitment to show up in underserved communities. We must listen to their concerns, include their voices, and communicate a clear and thoughtful message. We must also make the process easy if we hope to succeed in getting the COVID-19 vaccine to the communities that have been disproportionately impacted by the virus.












